Mood Swings, Anger, and Feeling “Off”: Why Menopause Affects More Than Your Body
Why Do I Feel Like a Stranger to Myself?
Many women entering perimenopause or menopause describe a disorienting sense of not feeling like themselves. Suddenly, patience is thinner, small frustrations spark outsized anger, and emotions swing rapidly from sadness to irritability.
These shifts aren’t a weakness of willpower or a lack of coping skills—they are rooted in real, measurable biological changes. Understanding what’s happening can help you reclaim both compassion for yourself and the tools to start feeling balanced again.
How Hormones Shape Mood
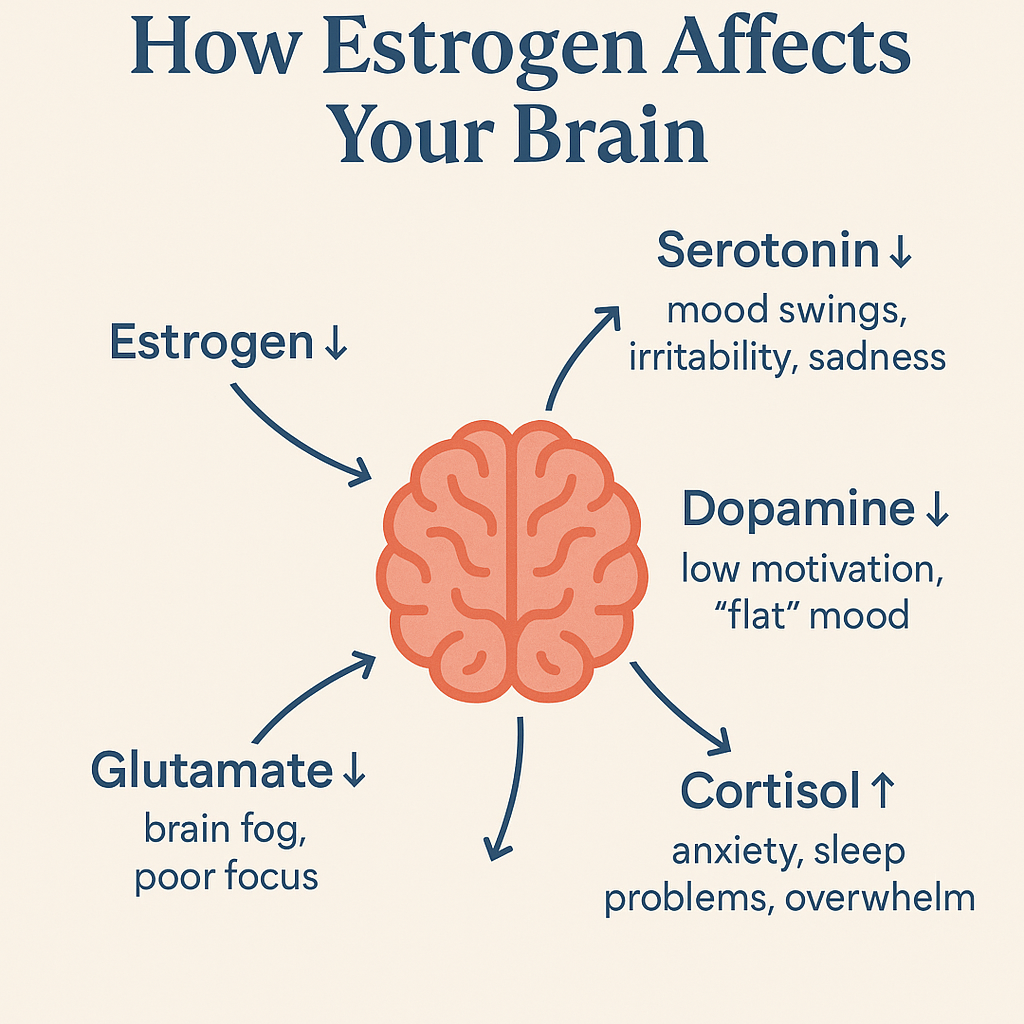
Estrogen doesn’t just regulate menstrual cycles—it has profound effects on the brain (1):
Serotonin: Supports emotional steadiness. Lower estrogen can mean lower serotonin, which is strongly linked to irritability, depression, and anxiety.
Dopamine: Involved in focus and motivation. Estrogen supports dopamine pathways, so its decline can leave you feeling unmotivated or “flat.”
Glutamate: A neurotransmitter critical for learning, memory, and mood regulation. Decreased estrogen weakens glutamate activity, affecting both cognition and emotional steadiness.
Cortisol: Estrogen helps keep cortisol (the stress hormone) in check. As estrogen levels drop, cortisol levels may rise, leading to feelings of overwhelm and increased emotional reactivity.
Common Emotional and Cognitive Symptoms
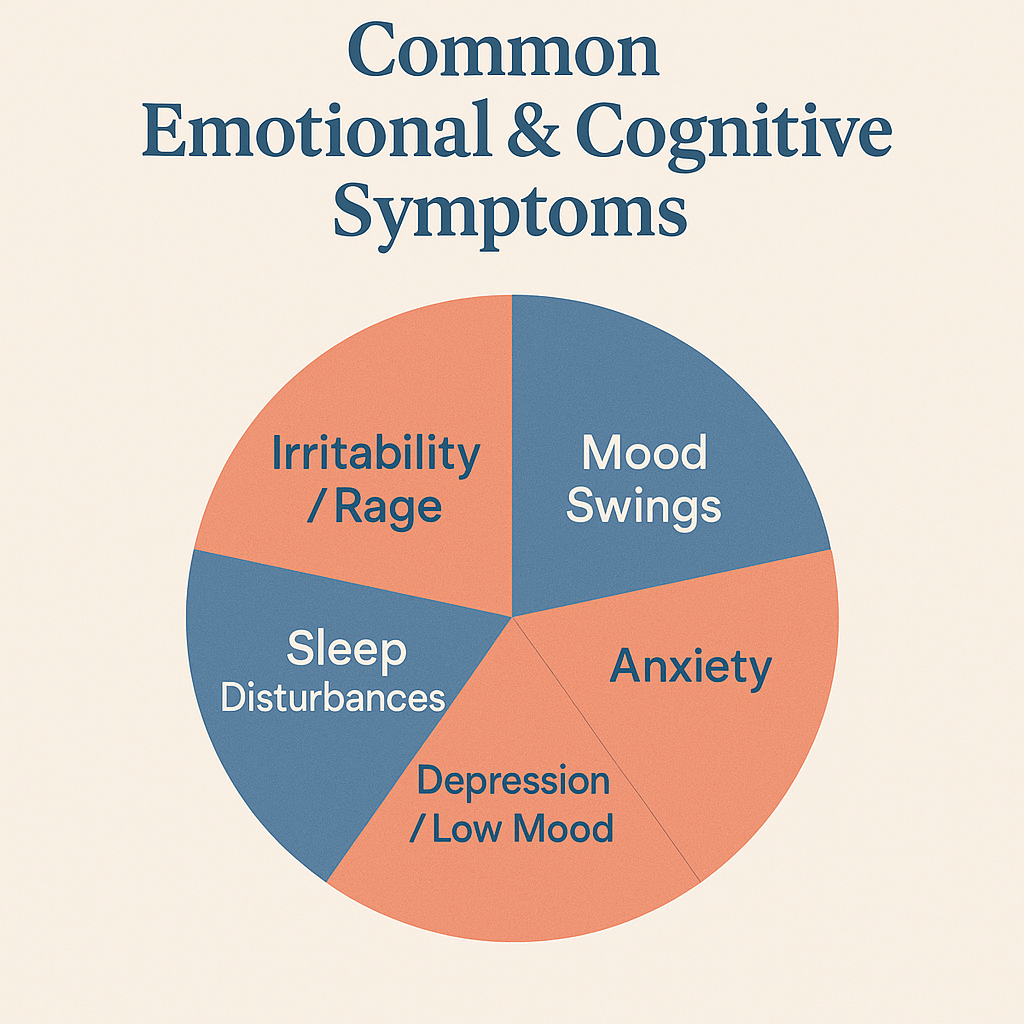
Women in perimenopause and menopause may experience:
Irritability & rage
Mood swings
Anxiety
Depression or low mood
Brain fog & forgetfulness
Sleep disturbances
Evidence-Based Treatments
Hormone Therapy
A 2025 retrospective cohort study of 920 peri- and postmenopausal women demonstrated that initiating or optimizing menopausal hormone therapy (MHT)—typically with estradiol (sometimes combined with progesterone or testosterone)—reduced symptom scores by nearly 45% within 107 days (2).
This shows that MHT can play a central role in restoring emotional balance, especially when symptoms are severe.
Lifestyle and Non-Medication Approaches
While hormones are often the root cause, lifestyle can influence how severe symptoms feel:
Exercise: Regular aerobic activity reduces depressive symptoms in midlife women (3).
Mindfulness & Meditation: Helps calm the nervous system and reduce stress reactivity (4).
Sleep Hygiene: Consistent routines and restorative sleep improve emotional resilience (5).
Nutrition: Omega-3s, whole grains, vegetables, and lean proteins support brain health (6).
The Empowered Wellness Approach
We know mood changes aren’t “just in your head.” That’s why we offer a whole-person model of care for women in perimenopause and menopause.
Step 1: Initial Care Consultation
Start with a conversation to share your story and goals.
Step 2: Comprehensive Lab Work
We order labs (through your insurance when possible) to assess hormone and health profiles.
Step 3: Personalized Care Plan
Your treatment plan may include MHT, other FDA-approved medications, and supportive strategies.
Step 4: Membership Program
Initial care consultation: We review labs and discuss a care plan that is personalized for you.
12-week intensive support: $800
Ongoing membership: $50/month
Medications and labs: billed through insurance when possible
New Add-On Services
Because mood and well-being are multi-layered, we now also offer à la carte services outside of our membership model:
Mental Health Counseling: One-on-one sessions with a licensed mental health counselor, focused on coping strategies, stress management, and emotional healing.
Nutrition Support with a Registered Dietitian: Personalized guidance to optimize diet for hormone balance, energy, and brain health.
These services can be added at any time, whether or not you’re enrolled in our membership program.
Menopausal mood changes are real, biologically driven, and deeply impactful—but they are not permanent, and they are not something you have to face alone. With evidence-based medical care, supportive counseling, and nutrition strategies, you can rediscover balance and start to feel like yourself again.
-
Turek J, Gąsior Ł. Estrogen fluctuations during the menopausal transition are a risk factor for depressive disorders. Pharmacol Rep. 2023;75(1):32-43. doi:10.1007/s43440-022-00444-2
Glynne S, Kamal A, McColl L, et al. Transdermal oestradiol and testosterone therapy for menopausal depression and mood symptoms: retrospective cohort study. Br J Psychiatry. Published online June 16, 2025. doi:10.1192/bjp.2025.101
Dugan SA, Bromberger JT, Segawa E, Avery E, Sternfeld B. Association between physical activity and depressive symptoms: midlife women in SWAN. Med Sci Sports Exerc. 2015;47(2):335-342. doi:10.1249/MSS.0000000000000407
Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. 2011;31(6):1041-1056. doi:10.1016/j.cpr.2011.04.006
Vandekerckhove M, Wang YL. Emotion, emotion regulation and sleep: An intimate relationship. AIMS Neurosci. 2017;5(1):1-17. Published 2017 Dec 1. doi:10.3934/Neuroscience.2018.1.1
Gómez-Pinilla F. Brain foods: the effects of nutrients on brain function. Nat Rev Neurosci. 2008;9(7):568-578. doi:10.1038/nrn2421